Migraine is the most common neurological disorder, and much has been learned about its mechanisms in recent years. However, the origin of painful impulses in the trigeminal nerve is still uncertain.
Our understanding of migraine disease has changed while there is much yet to learn. Let us review some of the most important principles about this medical condition…
Migraine is a disease of the nervous system. In the past, we believed that migraine headaches were caused by changes in blood vessels in the brain. Now it is clear that what happens in the brain is much more complicated.
The underlying problem with migraine sufferers is that their nervous system is too sensitive or too jumpy. It reacts to small or normal stimulation with an exaggerated response. Those triggers may be the result of something we consumed, excess stress, a lack of sleep or a change in the weather.
And how hypersensitive the nervous system is and what triggers the nervous system varies between people.
In other words migraine disease is not a single disease but a spectrum with symptoms ranging from mild and occasional to debilitating and daily.
Why is this? Genetics play a part in migraine disease.
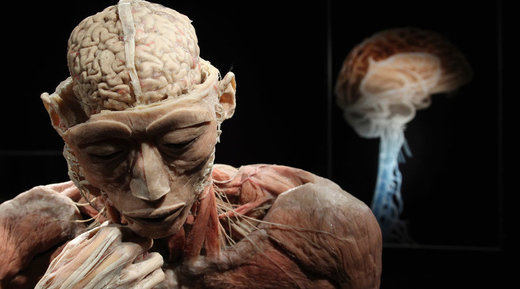
Let’s remind ourselves about how the nervous system works. If we look at what we think of as a nerve, we see how it is made up of a bundle of similar neurons.
Each individual neuron has a cell body with long extensions. When specialized sensors are stimulated, an electrical message starts on its way to the brain.
But it is actually the flow of the charged sodium ions into the cell through ion channels followed by the passing of potassium through separate ion channels out of the cell. That generates the electrical signal..
An electrical wave then moves rapidly towards the brain. At some point, each neuron reaches its limit and the signal must be transferred to the next set of neurons.

Calcium channels open and secondarily cause the release of chemicals called neurotransmitters into the synapses where receptors on the adjacent neurons must detect the neurotransmitters and regenerate the electrical signal.
It is during this complex process that mistakes can be made. Think of a genetic defect as a mixed up message about how the cell is to make things. For example, one of the known genetic defects of migraine is one where the cell is instructed to produce a protein that cannot fold into its normal three-dimensional shape.
When positioned in the cell membrane and an electric signal comes along, the defective protein may open up and let calcium ions into the cell. But it might not be able to snap back into a fully closed position allowing too much of the electrically charged calcium into the neuron.

In this case, the neuron would keep releasing neurotransmitters and the next cell would generate an exaggerated response. The consequence is that the neuron has overreacted to a stimulus. This is not just theoretical. There are known genetic defects of ion channels in families who suffer from migraine. Additionally, research has revealed genetic mistakes affecting how neurotransmitters are made, released and inactivated. Therefore, each individual inherits a mixture of genetic errors. This may partly explain the broad spectrum of migraine symptoms and how between individuals.

Migraine might affect a lot of different parts of the nervous system not just the pain pathways.
The trigeminal nerve has branches that innervate facial muscles, temporal mandibular joint, paranasal sinuses and teeth. When stimulated, branches of the trigeminal nerve transmit information back to the brain through the trigeminal nucleus in the brainstem. From brainstem, this message is sent to other parts of the conscious brain that acknowledge the pain and the need for action.
But for a migraine sufferer, the threshold for initiating this distress signal is lower than normal and the amplitude of the warning is abnormally high.

Cortical Spreading Depression
So, What causes the intense headache of migraine?
The current theory is that a trigger either in the brain stem or in periphery sets off an abnormal electrical event called a cortical spreading depression. This is a wave of electrical activity that sweeps slowly across the surface of the cortex.
A cortical spreading depression first initiates flashing lights or abnormal smells followed by an intense headache. The electrical depolarization results in a release of neurotransmitters and other molecules that cause secondary inflammation.
A person then experiences light sensitivity, nausea, foggy thinking and fatigue for hours.
By mechanisms that are still to be defined. The chemical reactions of a cortical spreading depression appear to affect the dura where blood vessels dilate and contract. Mast cells release their potent inflammatory chemicals and trigeminal nerve fibers send signals back to the brain stem.
Migraine medicine attempts to neutralize these chemicals.
While cortical spreading depressions cannot explain many of the symptoms of migraine disease. It is likely an important event in generating the most familiar, brief, intense experiences of migraine sufferers.

Migraine has a chronic form:
Central Sensitization
It has been observed that migraine sufferers have scarring within the brain. This may be a complication from the repeated inflammation associated with cortical spreading depressions or other migraine events within the brain.
Eventually parts of the damaged nervous system simply generate low-grade frequent unwelcome symptoms such as increased sensitivity to touch or light, daily headaches, tinnitus or diminished cognitive functions.
Central sensitization partly explains why migraine sufferers have different symptoms at different stages in their lives, also the damage to blood vessels from inflammation may explain the higher rates of stroke in migraine sufferers. And head trauma to the hypersensitive central nervous system may make migraine sufferers more vulnerable to chronic headache syndromes.
The Brain Stem may be the core of migraine disease. Another factor in migraine disease is that abnormal electrical activity of one set of neurons may affect the behavior of adjacent ones.

The Brain Stem is the crossroads of much of our brain circuitry. It is here that information controlling many body functions congregates in clusters of cell bodies called nuclei.
When electrical messages arrive in one nucleus they may be rerouted to other parts of the brain stem hypothalamus, thalamus and cortex. These nerve centres have exotic names such as the trigeminal nuclei, pulvinar nucleus, dorsal raphe and locus coeruleus.
While the trigeminal nucleus is the control center for headache pain. These adjacent nuclei controls stress, balance, mood, sleep and the autonomic system. An example is the generation of symptoms from the nasal and sinus region.
Many people mistake their chronic migraine symptoms for a recurring infection. In fact, one form of chronic migraine disease is where the trigeminal nucleus generates signals that the brain interprets as abnormal pressure or pain from within the paranasal sinuses, teeth or eyes.
Adjacent to the trigeminal nucleus is the superior salivatory nucleus. This nerve center controls the production of nasal secretions and the size of the turbinates within the nose.
A migraine sufferer not only feels sinus pressure but also experiences nasal congestion and the runny nose. The interplay between these nuclei may be another explanation for why some migraine sufferers have so many related symptoms many of which do not involve pain.

Female Hormones
Female hormones effect migraine disease. Sex hormones such as estrogen and progesterone have a profound but poorly understood effect on our nervous system. Sex hormones affect the nervous system of all women but for migraine sufferers their rise and fall throughout a lifetime helps to explain why the symptoms of migraine change so dramatically for women.
Estradiol better known as estrogen has a complicated role in our nervous system. For example, for any one neuron there are estradiol receptors on the nucleus as well as the surface of the cell. And, we know of genetic defects of both these receptors independent of the hormone receptors we know that estrogen also sensitizes our body to pain.
While we still have a lot to learn about sex hormones, we do know that they play a critical role in the waxing and waning of migraine disorders.
The several biological mechanisms that describe how migraine disorders occur explain why there are different strategies for treating migraine disease and why no one approach works for everyone.